
Cyclical spirals of hope and devastation are inherently tethered to recurrent pregnancy loss, like an unwanted encore that refuses to end. Having a pregnancy test light up with a positive, only to have it undone a few weeks later can be heartbreaking. Recurrent miscarriages usually stem from anatomic abnormalities, hormonal imbalances, chromosomal anomalies or blood coagulation.
However, while these factors are known to contribute to repeated spontaneous abortion, there is much that is unknown about the condition. With vigilant monitoring and careful testing, deterrent influences can be diagnosed and addressed, allowing a pregnancy to reach full term.

About one-third of pregnant women experience some form of bleeding or cramping during the first trimester. About 10% of known pregnancies end in miscarriage. Miscarriage is most commonly a result of a genetic abnormality in the embryo, a mechanism instituted by the body to prevent a pregnancy from progressing further. Of course, a genetic anomaly is a fluke occurrence and doesn't necessarily mean that a subsequent pregnancy will follow suit.
A miscarriage, therefore, is not indicative of a health problem, because most couples that miscarry go on to have healthy babies without any fertility intervention. When miscarriages become recurrent, there are chances that the underlying cause extends beyond just genetic anomalies. A timely diagnosis can help in breaking the cycle.
To Consult: Best Fertility Specialist in Mumbai
Two or more consecutive miscarriages is termed as recurrent pregnancy loss. The chances of experiencing another miscarriage in such a case rise marginally, from 15% to 35%, but the odds of pregnancy going smoothly are still high. Women over the age of 35 are more likely to miscarry. When it comes to repeated miscarriages, there are some factors that are known to play a significant role:
Chromosomal anomalies
Hormonal imbalances
Polycystic ovarian syndrome
Autoimmune disorders
Antiphospholipid antibodies
Uterine abnormalities
Unhealthy lifestyle
Poor ovarian reserve
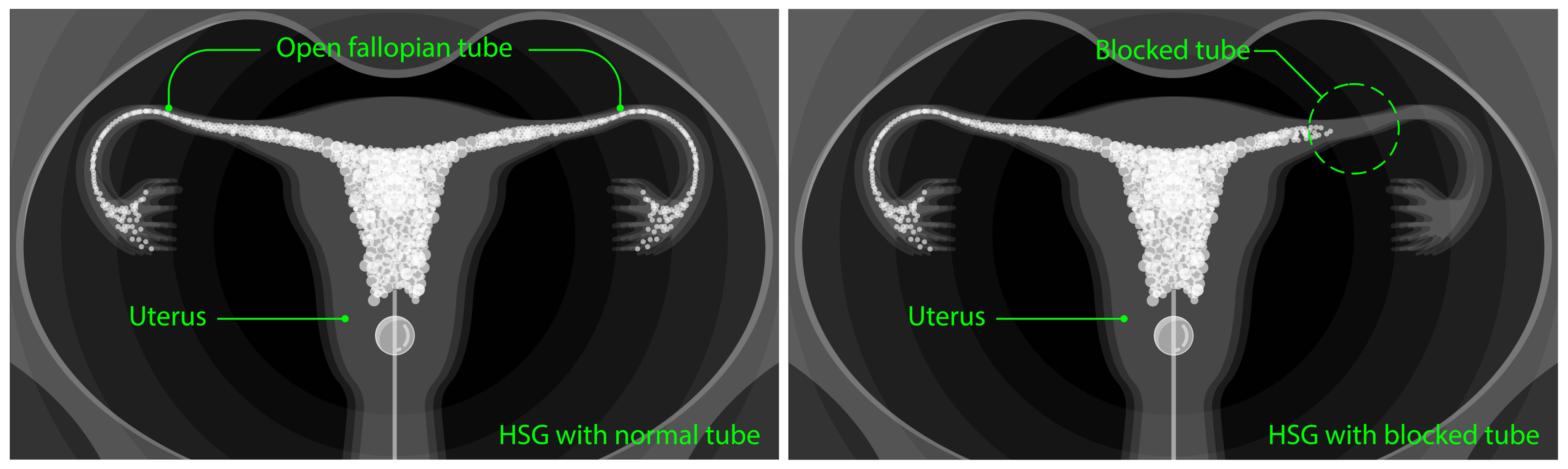
There's no treatment set in stone for recurrent pregnancy loss. Every case is different, with unique factors at play in each one. To begin with, your doctor may advise a range of tests, including a hysterosalpingogram to check your uterus, blood tests to screen for antiphospholipid antibodies and a karyotype to evaluate chromosomal abnormalities in you and your partner. Based on findings, your doctor may advise a route that is likely to produce favourable results. Speak to a doctor on Cloudnine to have yourself evaluated if you've been struggling with maintaining pregnancies. Advanced technologies in In vitro fertilisation (IVF) have opened new avenues for couples who have had repeated miscarriages. The sooner you seek medical help, the sooner you can fix the problem.

Miscarriages are hushed, dismissed and forgotten all too easily by society. For you, as parents, grieving a lost soul is an important process in the anticipation of your next new life. Allow yourself to be enveloped in anger, frustration, grief and sadness. Give yourself time to seek closure and let your wounds heal before you open your heart to a new baby. Communicate with your partner about how you're feeling and gain comfort in knowing that you're not alone on this journey. Bank on your inner circle of family and friends to vent your feelings. Support groups are an excellent way to connect with women experiencing similar pregnancy loss. Draw from their experiences and offer them yours.

On Cloudnine, our clinical ecosystem is equipped to offer you a clear-cut diagnosis that will pave the way for a definitive treatment plan. Our solutions are tailor-made and thoughtful, giving you the chance to take reign of your pregnancy spirals. On Cloudnine, trust us to help you reach the finish line.
Must Read: SURROGACY AND GESTATIONAL SURROGACY